Bless Us Every One
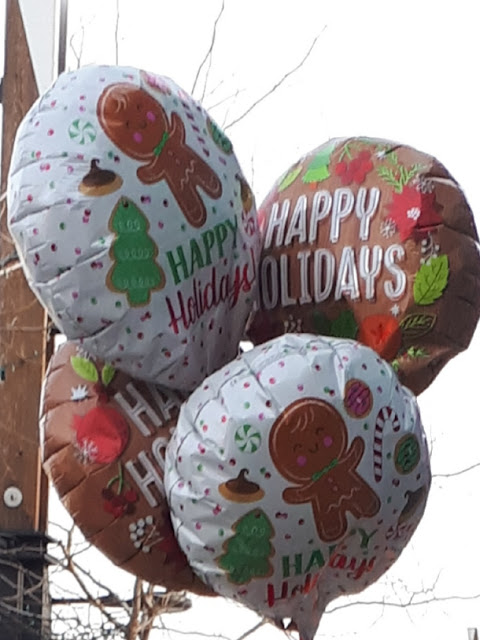
Yesterday I received an early Christmas gift in the form of a humbling experience. As I walked out the door of a downtown card shop, a person walked past dressed in a rather outlandish outfit. A pair of cut-off lycra shorts were pulled over a pair of shiny taupe tights. They wore a rainbow wig whose luscious waves tumbled hallway down the back of a red hoodie. Atop the wig they sported a pair of short white bunny ears. A blue suede purse rested on one hip and three large but flat Christmas gift bags dangled from the opposite arm. A bouquet of festive mylar balloons tied with red curling ribbon and covered in Christmas cookies and holiday wishes floated above them. I followed behind snapping a photo and rationalizing the invasion by the fact you couldn’t see their face. We met up at the corner and while we waited for some cars to pass I remembered today’s Random Act of Kindness. “Start-up a friendly chat”. “Are you Santa’s Christmas bunny?” I asked

